Inflammation of the prostate gland is one of the main urological problems in men under 50 years of age. Ten to twelve percent of all representatives of the stronger sex have experienced symptoms of prostatitis at least once in their lives. The disease can occur in acute and chronic form, on which its signs and symptoms directly depend.
What is prostatitis
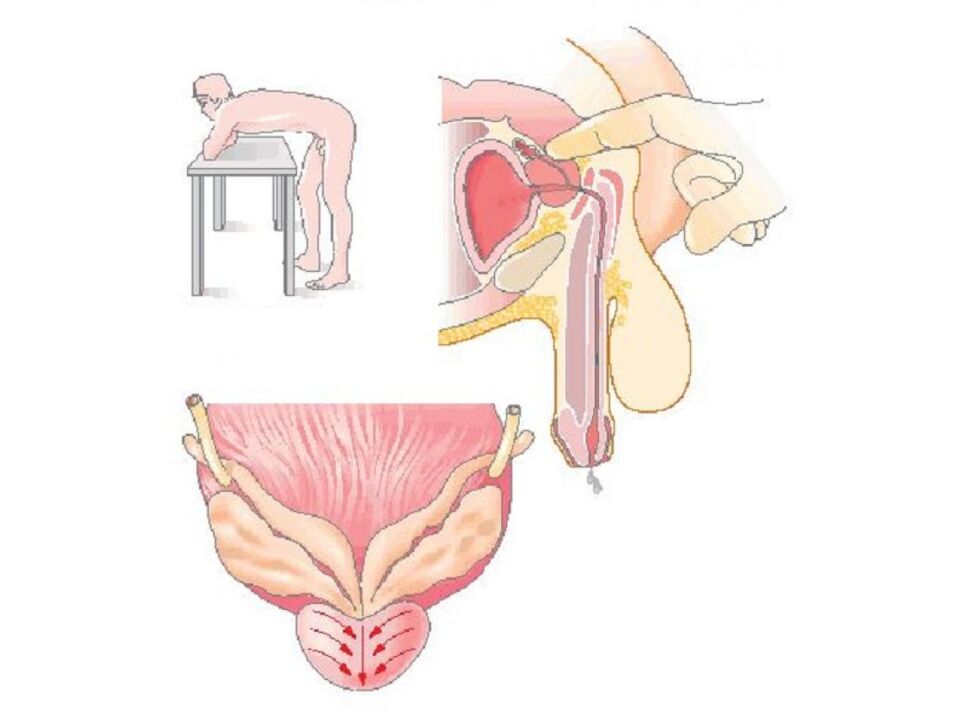
Prostatitis is a term meaning inflammation of the prostate gland.The prostate gland, or prostate, is an organ of the male reproductive system. Its normal size does not exceed the size of a walnut. The gland is located under the bladder, in front of the rectum. The prostate surrounds the urethra, the tube through which urine and semen exit the body. Its main function is the production of secretion (prostatic juice), which supports the vital activity of sperm after ejaculation.
The inflammatory process in the prostate gland can be caused by infection, as well as various other reasons.
Types and first signs of the disease
The first signs and further symptoms will depend on the type of prostatitis. In total, clinicians distinguish 4 varieties.
- Acute bacterial prostatitis: Caused by a bacterial infection, usually has a sudden onset that may resemble flu-like symptoms. This is the least common of the four types of prostatitis.
- Chronic bacterial prostatitis: Characterized by recurrent bacterial infections of the prostate gland. There may be little or no symptoms between attacks, which is also why it can be difficult to treat successfully.
- Chronic prostatitis/chronic pelvic pain syndrome: Most cases of prostatitis fall into this category, but at the same time this type is the least understood. It can be characterized as inflammatory or non-inflammatory, depending on the presence or absence of infection-fighting cells - antibodies in urine, semen and prostate secretions. It is often impossible to determine a single specific cause. Symptoms may come and go or remain intermittent.
- Asymptomatic inflammatory prostatitis: This disease is often diagnosed incidentally during treatment for infertility or prostate cancer. Persons with this form of prostatitis have no complaints of symptoms or discomfort, however, tests show the presence of infectious cells in the prostate secretion.
Main symptoms
Symptoms associated with prostatitis can vary depending on the underlying cause of the disease.Common, gradually increasing symptoms include:
- pain or burning when urinating (dysuria);
- difficulty urinating, such as a thin stream of urine or sluggish, intermittent urine;
- frequent urination, especially at night (nocturia - going to the toilet more than 2 times a night);
- urgent urge to urinate.
An important symptom is pain, which can occur or radiate to various areas of the lower body. She may be:
- in the rectum (rectal), sometimes combined with constipation;
- in the abdomen and/or lower back;
- in the perineum - between the scrotum and rectum.
Patients often report discomfort in the penis and testicles. Painful ejaculation is characteristic, and, in addition, prostatitis can be accompanied by sexual dysfunction.
A rapid and severe onset is usually characteristic of the acute bacterial form, which is distinguished by an additional symptom complex similar to that which occurs during the influenza virus.This:
- fever and chills;
- general malaise and body aches;
- enlarged lymph nodes;
- a sore throat.
If the patient ignores the first signs of the disease and does not seek help from a urologist-andrologist, then there are dangerous cases of purulent complications. Acute infectious prostatitis can develop into a severe form of pathology, when the prostate tissue becomes covered with pustules or abscesses. Symptoms include the following:
- cloudy urine or blood in the urine;
- discharge from the urethra;
- bad smell of urine and discharge.
If he detects initial signs of inflammation, a man should immediately consult a doctor for further diagnosis.
Diagnostic methods
Prostatitis is usually diagnosed through laboratory testing of a urine sample and examination of the prostate gland by a urologist.This examination involves palpation of the prostate through the rectum to examine any abnormalities. Sometimes the doctor collects and tests a sample of prostate secretions. To obtain it, the urologist massages the gland during a rectal examination. Because there is concern that the procedure may release bacteria into the bloodstream, this test is contraindicated in cases of acute bacterial prostatitis.
The urologist also measures body temperature in the armpit and rectally, then comparing the results. During acute prostatitis, the temperature in the anus will differ upward by about 0. 5 degrees.
Lab tests
Laboratory tests that may be ordered include:
- clinical blood and urine analysis;
- bacterioscopy and culture of urine sediment and prostate secretion - examination of samples under a microscope for the presence of bacteria;
- a smear of discharge from the urethra (if discharge is present);
- determination of the level of prostate specific antigen (PSA).
If a clinical blood test shows an increased level of leukocytes (from 10-12 per field of view), this will indicate the presence of inflammation. Acute infectious prostatitis is characterized by an increase in neutrophils, a type of white blood cell whose main function is to destroy pathogenic bacteria. There is also a decrease in the level of eosinophils (below 1% of all leukocytes), another group of leukocytes that is responsible for protecting the body from proteins of foreign origin. The erythrocyte sedimentation reaction, or red blood cells, is another indicator of a general clinical blood test and also indicates the presence of a pathological process in the body if its value exceeds 10 mm/h. The rate of sedimentation of these blood cells increases with increasing concentration in the blood plasma of markers of the inflammatory process: fibrinogen proteins and immunoglobulins, as well as C-reactive protein.
Bacterioscopy of urine sediment and prostate secretion will indicate the presence and number of pathological microorganisms in these biological fluids, and thanks to culture for sensitivity to antibiotics, the type of bacteria will be established for further selection of treatment. The causative microorganism can be determined, among other things, by taking a smear of discharge from the urethra for microscopic examination.
The prostate specific antigen test is a screening test in the form of an intravenous blood test for a protein that is produced exclusively by prostate cells. The protein norm depends on the age of the man and ranges from 2. 5 ng/ml for ages 41–50 years to 6. 5 ng/ml for men over 70 years of age. An increase in the level of this protein above the age norm means the need for a biopsy - tissue analysis for oncology. However, excess protein content can also be observed due to inflammation of the prostate gland.
PSA levels may also increase slightly with benign enlargement (adenoma) of the prostate and as a result of urinary tract infections.
Age-related PSA norms - table
| Age category | PSA norm |
|---|---|
| Under 40 years old | less than 2. 5 ng/ml |
| 40–49 years old | 2. 5 ng/ml |
| 50–59 years old | 3. 5 ng/ml |
| 60–69 years old | 4. 5 ng/ml |
| Over 70 years old | 6. 5 ng/ml |
Instrumental studies
Since none of the tests or analyzes individually provides a complete guarantee of a correct diagnosis, other methods - instrumental ones - can be used as part of a comprehensive diagnosis. These include:
- Urodynamic study of the bladder- a complex instrumental method using special equipment allows you to determine whether the bladder is completely emptied, the rate of urine flow, the pressure inside the bladder and urethra, and also to assess the effect of prostatitis on normal urination. This study is recommended for people with chronic urinary problems: intermittent or thin stream, incontinence, frequent urination, etc. It is also indicated for patients with prolonged inflammation of the prostate gland, especially when standard therapy is ineffective. Before the examination, a special catheter-sensor is inserted into the patient's urethra in a horizontal position, which is also connected to measuring equipment. Next, he is asked to drink a certain amount of clean water, simultaneously recording the feeling of a full bladder, the first urge to urinate, the presence of urine leaks, etc. Then the patient is transferred to a specially equipped chair, on which he will need to relieve himself while still under the control of sensors andequipment that makes the necessary measurements. The procedure consists of several stages, each of which takes about half an hour. The results of the urodynamic study are given to the patient immediately after its completion.
- Ultrasound Imaging (US)- the method is used as a diagnosis of existing disorders, and it is also indicated for men after 45 years of age annually as a prevention of prostatitis and other gland diseases. The study is carried out in the morning on an empty stomach using an ultrasound machine through the anterior abdominal wall with a bladder filled with clean water, as well as by inserting a special sensor 5–7 cm deep into the rectum (rectal method) or through the urethra. The procedure is absolutely safe and allows you to determine the contour, size and condition of individual areas of the prostate gland. The volume of a healthy prostate is approximately 20–25 cm3. The maximum length, width and thickness are 3. 5 cm, 4 cm and 2 cm respectively.
- Magnetic resonance imaging (MRI)- the method allows you to study in detail the structure, density, condition and even blood flow of the prostate; sometimes, for a better overview, an additional contrast agent is injected intravenously. The examination is also carried out to differentiate prostatitis from oncology. An MRI machine is a large cylinder surrounded by a magnet, into which a medical table with a patient slides inside, like a tunnel. The person should wear loose clothing without metal fittings and refrain from heavy food 10–12 hours before the procedure. Before the examination, it is imperative to remove watches, jewelry, and any other metal objects. If the patient has metal-containing implants or cardiac devices in the patient’s body, the MRI diagnostic method is contraindicated. To carry out the procedure, a transrectal sensor is most often used (although it is possible without it), having previously cleaned the rectum with an enema. The nurse inserts the sensor and secures it with a special disposable cuff. During the entire duration of the examination, which is about 30 minutes, the patient should lie as still as possible. The procedure is painless.
- Cystoscopy- examination of the mucous membranes of the urethra and bladder using a cystoscope - a long narrow catheter with a light bulb and a camera at the end under local anesthesia. The procedure is carried out after the bladder is full. The duration of cystoscopy is about 15 minutes. The method allows you to assess the condition of the urinary tract, excluding other possible diseases that cause problems with urination.
- Prostate biopsy- is a necessary procedure if, after a comprehensive examination, the doctor suspects a malignant process in the prostate. It must be excluded or confirmed to select treatment tactics. The procedure is performed on an outpatient basis by inserting a puncture needle through the patient's rectum and taking a sample of prostate tissue. A local anesthetic is injected into the anus, then, when it has taken effect, an ultrasound probe with a needle attachment is inserted into the intestine. Under ultrasound guidance, the surgeon determines the places from which it is necessary to "pinch off" material for analysis. Typically there are up to 18 different points on the organ. The biopsy does not cause pain; after the anesthesia wears off, only slight discomfort is possible.

%20and%20inflamed%20(right)%20prostate%20on%20MRI%20images.jpg)
If a patient experiences recurring episodes of urinary tract infection and prostatitis, the specialist will prescribe a full comprehensive examination of the genitourinary system to identify anatomical abnormalities.
Differential diagnosis
Acute prostatitis symptoms may resemble inflammation of the bladder or urethra. In all cases, symptoms include painful and frequent urination. But acute prostatitis is distinguished by vivid symptoms of general intoxication and an admixture of pus in the urine and secretions. Palpation examination of the prostate will be painful and will reveal an increase in the size of the gland, which will not happen with cystitis or urethritis.
Doctors say prostate inflammation does not increase the risk of prostate cancer.
Chronic inflammation of the prostate gland should be differentiated in young men with anogenital symptom complex and vegetative urogenital syndrome. These diseases can only be distinguished by analyzing prostate secretions for the presence of bacteria. In men over 45 years of age, it is necessary to exclude oncology and prostate adenoma, which in the initial stages are most often asymptomatic, unlike inflammation of the prostate. For a more detailed analysis, the urologist will prescribe a PSA test, and then, if necessary, a biopsy.
Prostatitis can be an acute bacterial disease, which is often easily treated with antibiotics, or a chronic disease that recurs and requires constant medical monitoring and control. In each case, only a specialist in the field of urology and andrology can correctly diagnose the disease.





























